Generic drug of the Therapeutic class: Cardiology and angiology
Active ingredients: Olmesartan medoxomil , Amlodipine
what is AXELER ?
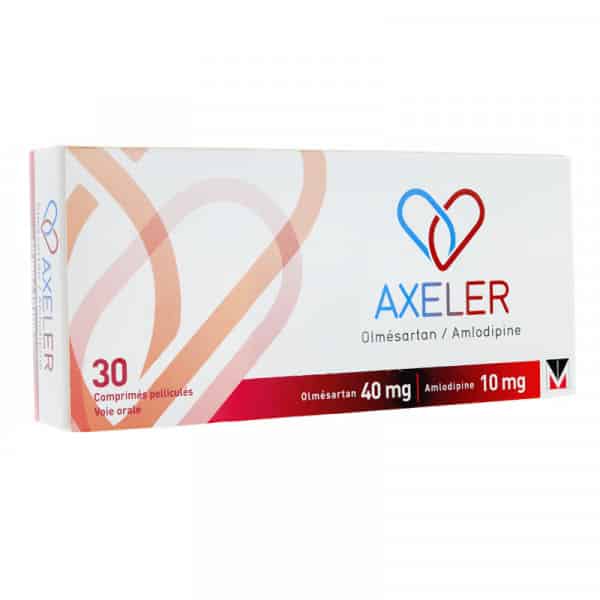
AXELER 40 MG / 10 MG: GENERAL INFORMATION
AXELER is used to treat high blood pressure (hypertension) in patients whose blood pressure is not adequately controlled with either olmesartan medoxomil or amlodipine, each given alone.
PRESENTATION (S) AVAILABLE FOR AXELER 40 MG / 10 MG
3 presentations are available for this drug:
- polyamide aluminum PVC-Aluminum blister pack (s) of 30 tablet (s)
- polyamide aluminum PVC-Aluminum blister pack (s) of 50 tablet (s)
- polyamide aluminum PVC-Aluminum blister pack (s) of 90 tablet (s)
| FEATURE | DESCRIPTION |
| Pharmaceutical class | substances that affect the renin-angiotensin system |
| Active substance (s) | for one tablet: olmesartan medoxomil (40 mg), amlodipine besilate (13.888 mg) |
| General medicine | no |
| Pharmaceutical form | coated tablet |
| Route (s) of administration | oral |
| Social security reimbursement rate | 65% |
| Laboratory (s) | MENARINI FRANCE |
| Conditions of issue | available by simple prescription |
what is AXELER medication used for and indication?
- Treatment of essential hypertension.
- Axeler is indicated in adult patients whose blood pressure is not adequately controlled on olmesartan medoxomil or amlodipine monotherapy ( see sections Dosage and Administration and Pharmacodynamic properties ).
AXELER Dosage
Dosage
Adults
- The recommended dose of AXELER is one tablet per day.
- AXELER can be used in patients whose blood pressure is not adequately controlled by AXELER 20 mg / 5 mg.
- A gradual adjustment of the dose of each component is recommended before switching to the fixed dose combination. A direct switch from monotherapy to a fixed dose combination may be considered if it is clinically justified.
- For convenience, patients taking olmesartan medoxomil and amlodipine separately as tablets may instead take the dosage of AXELER tablet corresponding to the same doses of these two components.
- AXELER can be taken with or without food.
Elderly subjects (65 years and over)
- In most cases, no dosage adjustment of the recommended dose is necessary in the elderly, but any increase in dosage should be done with caution ( see sections 4.4 and Pharmacokinetics ). If an increase to the maximum dose of 40 mg olmesartan medoxomil per day is necessary, blood pressure should be closely monitored.
Renal failure
- In patients with mild to moderate renal impairment (creatinine clearance 20-60 ml / min), the maximum dose of olmesartan medoxomil is 20 mg once daily, taking into account the limited experience of patients. higher dosages in this group of patients.
- In patients with severe renal impairment (creatinine clearance <20 ml / min) the use of AXELER is not recommended ( see sections 4.4 and Pharmacokinetic properties ). In patients with moderate renal impairment, it is advisable to monitor potassium and creatinine levels.
Hepatic insufficiency
- AXELER should be used with caution in patients with mild to moderate hepatic impairment ( see sections 4.4 and Pharmacokinetic properties ).
- In patients with moderate hepatic impairment, the recommended starting dose of olmesartan medoxomil is 10 mg once daily and the maximum dose is 20 mg once daily.
- Close monitoring of blood pressure and renal function is recommended in patients with hepatic impairment already treated with diuretics and / or other antihypertensive drugs. There is no experience with the use of olmesartan medoxomil in patients with severe hepatic impairment.
- As with any calcium channel blocker, the half-life of amlodipine is prolonged in patients with impaired hepatic function and dosage recommendations have not been established. Therefore, AXELER should be administered with caution in these patients. The pharmacokinetics of amlodipine have not been studied in severe hepatic impairment. Amlodipine should be started at the lowest dose and increased slowly in patients with severe hepatic impairment. The use of AXELER in patients with severe hepatic impairment is contraindicated .
Pediatric population
- The safety and efficacy of AXELER in children and adolescents below 18 years of age have not been established. No data is available.
Administration mode
- The tablet should be swallowed with a sufficient amount of liquid (eg a glass of water). The tablet should not be chewed and should be taken at the same time each day.
AXELER Contraindications
- Hypersensitivity to the active substances, to dihydropyridines or to any of the excipients (see section Composition ).
- 2 nd and 3 rd trimesters of pregnancy (see sections Warnings and precautions for use and Pregnancy and breast-feeding ).
- Severe hepatic impairment and obstruction of the bile ducts .
Due to the presence of amlodipine, AXELER is also contraindicated in patients with:
- Severe hypotension,
- shock (including cardiogenic shock),
- An obstruction of the outflow path of the left ventricle (for example high-grade aortic stenosis),
- Hemodynamically unstable heart failure after acute myocardial infarction.
How To Take AXELER?
- Always take this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if in doubt.
- The recommended dose of AXELER is one tablet per day.
- The tablets can be taken with or without food. Swallow the tablet with a liquid (such as a glass of water). The tablet should not be chewed. Do not take it with grapefruit juice. If possible, take your daily dose at the same time each day, for example at breakfast time.
how does AXELER work?
Pharmacotherapeutic group: angiotensin II antagonists and calcium channel blockers, ATC code: C09DB02.
Action mechanism
- AXELER combines an angiotensin II receptor antagonist, olmesartan medoxomil, with a calcium channel blocker, amlodipine besilate. The combination of these active substances has a synergistic antihypertensive effect, lowering blood pressure more significantly than each of the components administered alone.
Clinical efficacy and safety
AXELER
- In a double-blind, randomized, placebo-controlled, factorial trial including 1940 patients (71% of Caucasian origin and 29% of non-Caucasian origin) for 8 weeks, treatment with the different strengths of AXELER resulted in reductions significantly higher diastolic and systolic blood pressure compared to the respective monotherapies of the components. The mean reduction in systolic / diastolic blood pressure was dose-dependent: -24 / -14 mmHg (20 mg / 5 mg combination), -25 / -16 mmHg (40 mg / 5 mg combination) and -30 / -19 mmHg (combination 40 mg / 10 mg). AXELER 40 mg / 5 mg resulted in an additional reduction in systolic / diastolic blood pressure when sitting by 2.5 / 1.7 mmHg compared to AXELER 20 mg / 5 mg. Likewise, AXELER 40 mg / 10 mg resulted in an additional reduction in systolic / diastolic blood pressure when sitting by 4.7 / 3.5 mmHg compared to AXELER 40 mg / 5 mg. The proportion of patients achieving systolic and diastolic blood pressure target values (<140/90 mmHg in non-diabetic patients and <130/80 mmHg in diabetic patients) was 42.5%, 51.0% and 49.1% for AXELER 20 mg / 5 mg, for AXELER 40 mg / 5 mg and for AXELER 40 mg / 10 mg. Most of the antihypertensive effect of AXELER was usually achieved within the first 2 weeks of treatment. The proportion of patients achieving systolic and diastolic blood pressure target values (<140/90 mmHg in non-diabetic patients and <130/80 mmHg in diabetic patients) was 42.5%, 51.0% and 49.1% for AXELER 20 mg / 5 mg, for AXELER 40 mg / 5 mg and for AXELER 40 mg / 10 mg. Most of the antihypertensive effect of AXELER was usually achieved within the first 2 weeks of treatment. The proportion of patients achieving systolic and diastolic blood pressure target values (<140/90 mmHg in non-diabetic patients and <130/80 mmHg in diabetic patients) was 42.5%, 51.0% and 49.1% for AXELER 20 mg / 5 mg, for AXELER 40 mg / 5 mg and for AXELER 40 mg / 10 mg. Most of the antihypertensive effect of AXELER was usually achieved within the first 2 weeks of treatment.
- A second double-blind, randomized, placebo-controlled trial evaluated the effectiveness of adding amlodipine in patients of Caucasian origin whose blood pressure was insufficiently controlled with olmesartan medoxomil 20 mg as monotherapy for 8 weeks. In patients who continued to receive 20 mg olmesartan medoxomil alone, systolic / diastolic blood pressure was reduced by -10.6 / -7.8 mmHg after an additional 8 weeks of treatment. Addition of amlodipine 5 mg for 8 weeks resulted in a reduction in systolic / diastolic blood pressure of -16.2 / -10.6 mmHg (p = 0.0006).
- The proportion of patients reaching the target blood pressure values (<140/90 mmHg in non-diabetic patients and <130/80 mmHg in diabetic patients) was 44.5% with the 20 mg / 5 mg combination versus 28 , 5% with olmesartan medoxomil 20 mg alone.
- An additional trial evaluated the addition of different doses of olmesartan medoxomil in patients of Caucasian origin whose blood pressure was insufficiently controlled with amlodipine 5 mg as monotherapy for 8 weeks.
- In patients who continued to receive 5 mg amlodipine alone, systolic / diastolic blood pressure was reduced by -9.9 / -5.7 mmHg after an additional 8 weeks. Addition of olmesartan medoxomil 20 mg resulted in a reduction in systolic / diastolic blood pressure of -15.3 / -9.3 mmHg and addition of olmesartan medoxomil 40 mg resulted in a reduction in systolic blood pressure / diastolic of -16.7 / -9.5 mmHg (p <0.0001). The proportions of patients reaching blood pressure targets (<140/90 mmHg in non-diabetic patients and <130/80 mmHg in diabetic patients) were 29.9% in the group that continued to receive the amlodipine 5 mg alone, 53.5% with AXELER 20 mg / 5 mg and 50.5% with AXELER 40 mg / 5 mg.
- No randomized studies comparing, in uncontrolled hypertensive patients, the use of medium doses of AXELER versus increasing doses up to the maximum dose of amlodipine or olmesartan as monotherapy is not available.
- These 3 trials confirmed that the drop in blood pressure induced by AXELER administered once daily is maintained over 24 h, with valley-peak ratios of 71% to 82% for systolic and diastolic responses and efficacy out of 24. h was confirmed by outpatient blood pressure measurement.
- The antihypertensive effect of AXELER is the same regardless of age and sex, and whether or not patients have diabetes.
- In 2 extensions of open-label and non-randomized trials, maintenance of the efficacy of AXELER 40 mg / 5 mg has been demonstrated at one year in 49 to 67% of patients.
Olmesartan medoxomil (active ingredient in AXELER)
- Olmesartan medoxomil, a component of AXELER, is a selective angiotensin II (AT1) type 1 receptor antagonist. Olmesartan medoxomil is rapidly transformed into the pharmacologically active metabolite, olmesartan. Angiotensin II is the main vasoactive hormone of the renin-angiotensin-aldosterone system. It plays an important role in the pathophysiology of hypertension. The effects of angiotensin II are vasoconstriction, stimulation of the synthesis and release of aldosterone, cardiac stimulation and renal sodium reabsorption. Olmesartan blocks the vasoconstrictor effects of angiotensin II and those related to the secretion of aldosterone by blocking its binding to AT1 receptors present in tissues such as vascular smooth muscles and adrenal glands. The effect of olmesartan is independent of the origin or the route of synthesis of angiotensin II. Selective antagonism of angiotensin II (AT1) receptors by olmesartan results in increased plasma renin levels and angiotensin I and II concentrations, as well as decreased plasma concentrations of aldosterone.
- In hypertensive patients, olmesartan medoxomil causes a dose-dependent and lasting decrease in blood pressure. No hypotension related to the first dose, no case of tachyphylaxis during prolonged administration, nor any rebound effect on abrupt discontinuation of treatment were observed.
- In hypertensive patients, administration of a daily dose of olmesartan medoxomil produces a gradual and effective decrease in blood pressure over 24 hours. At an equivalent total daily dose, administration in 1 or 2 doses results in the same decrease in blood pressure.
- With continuous treatment, the maximum decrease in blood pressure is achieved 8 weeks after the start of treatment, although a significant drop in blood pressure is already observed after 2 weeks of treatment.
- The effect of olmesartan medoxomil on mortality and morbidity is not yet known.
- The ROADMAP study (Randomized Olmesartan and Diabetes Microalbuminuria Prevention study, Study evaluating olmesartan medoxomil in the prevention of microalbuminuria in type II diabetic patients) carried out in 4447 patients with type 2 diabetes, normoalbuminuria and having at least an additional cardiovascular risk factor, assessed whether treatment with olmesartan medoxomil could delay the onset of microalbuminuria. During a median follow-up period of 3.2 years, patients received olmesartan medoxomil or placebo in addition to other antihypertensive drugs, except angiotensin II converting enzyme inhibitors and angiotensin II receptor antagonists.
- For the primary endpoint, the study demonstrated a significant reduction in the time to onset of microalbuminuria, in favor of olmesartan medoxomil. After adjusting for blood pressure level, this risk reduction was no longer statistically significant. 8.2% (178 out of 2160) of patients in the olmesartan medoxomil group and 9.8% (210 out of 2139) of patients in the placebo group developed microalbuminuria.
- For secondary endpoints, cardiovascular events occurred in 96 patients (4.3%) on olmesartan medoxomil and in 94 patients (4.2%) on placebo. The incidence of cardiovascular mortality was higher with olmesartan medoxomil compared to placebo (15 patients (0.7%) versus 3 patients (0.1%)), despite similar rates of non-fatal stroke (14 patients (0.6%) versus 8 patients (0.4%)), non-fatal myocardial infarction (17 patients (0.8%) versus 26 patients (1.2%)) and mortality non-cardiovascular (11 patients (0.5%) versus 12 patients (0.5%)). The overall mortality with olmesartan medoxomil was increased in number of cases (26 patients (1.2%) versus 15 patients (0.7%)), mainly due to a higher number of fatal cardiovascular events.
- The ORIENT study (Olmesartan Reducing Incidence of End-stage Renal disease in Diabetic Nephropathy Trial, Study to evaluate olmesartan medoxomil in secondary prevention in diabetic patients with nephropathy) evaluated the effects of olmesartan medoxomil on renal and cardiovascular events in 577 patients, randomized, Japanese and Chinese, with type 2 diabetes with established nephropathy. During a median follow-up period of 3.1 years, patients received olmesartan medoxomil or placebo in addition to other antihypertensive drugs, including angiotensin II converting enzyme inhibitors.
- The primary composite endpoint (time to onset of first event of serum creatinine doubling, end stage renal disease and all-cause death) occurred in 116 patients in the olmesartan medoxomil group (41.1%) and in 129 patients in the placebo group (45.4%) (HR 0.97 (95% CI [0.75 to 1.24]); p = 0.791). The composite secondary cardiovascular endpoint occurred in 40 patients treated with olmesartan medoxomil (14.2%) and 53 patients treated with placebo (18.7%). This composite cardiovascular endpoint included cardiovascular deaths in 10 (3.5%) patients receiving olmesartan medoxomil versus 3 (1.1%) patients receiving placebo, overall mortality in 19 (6.7%) patients versus 20 (7.0%), non-fatal stroke in 8 (2.8%) patients versus 11 (3,
Amlodipine (active ingredient in AXELER)
- Amlodipine, a component of AXELER, is a calcium channel blocker that inhibits transmembrane entry of calcium ions through potential-dependent L-type channels in heart muscle and vascular smooth muscle. Experimental data indicate that amlodipine binds to both dihydropyridine and non-dihydropyridine binding sites. Amlodipine has a relatively selective effect at the vessel level, with a greater effect on vascular smooth muscle cells than on cardiac muscle cells. The antihypertensive effect of amlodipine results from a direct relaxing effect at the level of vascular smooth muscle, which leads to a reduction in peripheral resistance and, therefore, in blood pressure.
- In hypertensive patients, amlodipine causes a dose-dependent and lasting decrease in blood pressure. No hypotensive effect associated with the first dose, nor tachyphylaxis in the event of prolonged administration has been described. No rebound effect upon abrupt discontinuation of treatment was observed.
- After administration of therapeutic doses to hypertensive patients, amlodipine results in an effective reduction in blood pressure when lying, sitting or standing. Long-term use of amlodipine is not associated with a significant change in heart rate or in plasma catecholamine levels. In hypertensive patients with normal renal function, therapeutic doses of amlodipine decrease renal vascular resistance and increase glomerular filtration rate as well as efficient renal plasma flow, without modification of filtration fraction or proteinuria.
- In hemodynamic studies in patients with heart failure and in clinical trials based on stress tests in patients with NYHA stage III to IV heart failure, amlodipine did not cause of clinical deterioration as evidenced by resistance exercise, left ventricular ejection fraction, and by clinical signs and symptoms.
- A placebo-controlled study (PRAISE) designed to evaluate patients with NYHA-classified stage III to IV heart failure receiving digoxin, diuretics and angiotensin converting enzyme inhibitors , showed that amlodipine did not increase the risk of mortality or the combined risk of mortality and morbidity in these patients with heart failure.
- In a long-term, placebo-controlled, follow-up study (PRAISE-2) evaluating amlodipine in patients with stage III to IV heart failure according to the NYHA classification without clinical symptoms or objective findings suggestive of underlying ischemia, treated with stable doses of angiotensin converting enzyme inhibitors, digitalis, and diuretics, amlodipine had no effect on total or cardiovascular mortality. In this same population, amlodipine was associated with an increase in reported cases of pulmonary edema, although the difference in the incidence of worsening heart failure was not significant compared to placebo.
Study on the preventive treatment of heart failure (Treatment to Prevent Heart Attack Trial, ALLHAT)
- The ALLHAT (Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial), randomized, double-blind, morbidity and mortality study was performed to compare treatments recent: amlodipine 2.5 to 10 mg / day (calcium channel blocker) or lisinopril 10 to 40 mg / day (ACE inhibitor) as first-line treatment compared to a thiazide diuretic, chlortalidone at a dose of 12, 5 to 25 mg / day in mild to moderate hypertension.
- A total of 33,357 hypertensive patients aged 55 or over were randomized and followed for an average of 4.9 years. Patients had at least one risk factor for additional coronary artery disease, including: history of myocardial infarction or stroke (more than six months prior to inclusion) or documentation of other atherosclerotic cardiovascular disease (in total 51.5%), type 2 diabetes (36.1%), HDL cholesterol <35 mg / dl (11.6%), left ventricular hypertrophy diagnosed by electrocardiography or echocardiography (20.9%), current smoking (21 , 9%).
- The primary composite endpoint was fatal coronary artery disease or non-fatal myocardial infarction. No significant difference was observed in the primary endpoint between treatment with amlodipine and treatment with chlortalidone: RR 0.98; 95% CI [0.90 to 1.07]; p = 0.65. Among the secondary endpoints, the incidence of heart failure (part of a composite cardiovascular endpoint) was significantly higher in the amlodipine group compared to the chlortalidone group (10.2% versus 7, 7%; RR: 1.38; 95% CI [1.25 to 1.52]; p <0.001). However, no significant difference in mortality from any cause was observed between treatment with amlodipine and treatment with chlortalidone: RR: 0, 96; 95% CI [0.89 to 1.02]; p = 0.20.
Other information
- The use of the combination of an ACE inhibitor with an angiotensin II receptor antagonist (ARAII) has been analyzed in two large randomized controlled trials (ONTARGET (ONgoing Telmisartan) Alone and in combination with Ramipril Global Endpoint Trial) and VA NEPHRON-D (The Veterans Affairs Nephropathy in Diabetes)).
- The ONTARGET study was performed in patients with a history of cardiovascular disease or cerebrovascular disease, type 2 diabetes with target organ damage. The VA NEPHRON-D study was performed in patients with type 2 diabetes and diabetic nephropathy.
- In comparison with monotherapy, these studies did not demonstrate a significant beneficial effect on the evolution of renal and / or cardiovascular damage and on mortality, while an increased risk of hyperkalaemia was observed. , acute renal failure and / or hypotension.
- These results are also applicable to other ACE inhibitors and ARBs II, given the similarity of their pharmacodynamic properties.
- ACE inhibitors and ARBs II should therefore not be combined in patients with diabetic nephropathy.
- The ALTITUDE study (Aliskiren Trial in Type 2 Diabetes Using Cardiovascular and Renal Disease Endpoints) was performed to assess the benefit of adding aliskiren to standard ACE inhibitor or ARB II therapy in patients with type 2 diabetes and chronic renal failure, with or without cardiovascular disorders. This study was terminated prematurely due to an increased risk of adverse events. Cardiovascular deaths and strokes were more common in the aliskiren group than in the placebo group; likewise adverse events and certain serious adverse events such as hyperkalaemia, hypotension and
How To Store AXELER?
- Keep this medication out of the sight and reach of children.
- Do not use this medicine after the expiry date which is stated on the pack and on the blister after EXP. The expiration date refers to the last day of that month.
- This product does not require any special storage conditions .
- Do not throw away any medicines via a wastewater treatment plant or with household waste. Ask your pharmacist how to throw away the medicines you no longer use. These measures will help protect the environment.
AXELER Side Effects
- The most frequently reported adverse reactions during treatment with AXELER are peripheral edema (11.3%), headache (5.3%) and dizziness (4.5%).
- The adverse reactions observed with AXELER in clinical trials, safety studies after marketing authorization and spontaneous reports are summarized in the table below, together with the adverse reactions reported with one of the components , olmesartan medoxomil and amlodipine, given the known safety profiles of these substances.
The following definitions have been used in order to rank the frequency of adverse reactions:
- Very common (≥ 1/10)
- Common (≥ 1/100 to <1/10)
- Uncommon (≥ 1/1000 to <1/100)
- Rare (≥ 1 / 10,000 to <1 / 1,000)
- Very rare (<1 / 10,000)
Not known (frequency cannot be estimated from the available data)
|
MedDRA System Organ Classes |
Side effects | Frequency | ||
| Olmesartan medoxomil / amlodipine combination | Olmesartan medoxomil | Amlodipine | ||
|
Blood and lymphatic system disorders |
Leukocytopenia |
Very rare |
||
|
Thrombocytopenia |
Rare |
Very rare |
||
|
Immune system disorders |
Allergic reaction / Hypersensitivity to the product |
Rare |
Very rare |
|
|
Anaphylactic reaction |
Rare |
|||
|
Metabolism and nutrition disorders |
Hyperglycemia |
Very rare |
||
|
Hyperkalaemia |
Rare |
Rare |
||
|
Hypertriglyceridemia |
Frequent |
|||
|
Hyperuricemia |
Frequent |
|||
|
Psychiatric disorders |
Confusion |
Rare |
||
|
Depression |
Rare |
|||
|
Insomnia |
Rare |
|||
|
Irritability |
Rare |
|||
|
Decreased libido |
Rare |
|||
|
Mood changes (including anxiety) |
Rare |
|||
|
Nervous system disorders |
Vertiginous sensations |
Frequent |
Frequent |
Frequent |
|
Dysgeusia |
Rare |
|||
|
Headache |
Frequent |
Frequent |
Common (especially at the start of treatment) |
|
|
Hypertonia |
Very rare |
|||
|
Hypoaesthesia |
Rare |
Rare |
||
|
Lethargy |
Rare |
|||
|
Paresthesia |
Rare |
Rare |
||
|
Peripheral neuropathy |
Very rare |
|||
|
Dizzying postural sensations |
Rare |
|||
|
Sleeping troubles |
Rare |
|||
|
Drowsiness |
Frequent |
|||
|
Syncope |
Rare |
Rare |
||
|
Tremors |
Rare |
|||
|
Eye disorders |
Visual disturbances (including diplopia) |
Rare |
||
|
Ear and labyrinth disorders |
Tinnitus |
Rare |
||
|
Dizziness |
Rare |
Rare |
||
|
Cardiac disorders |
Angina pectoris |
Rare |
Uncommon (including worsening of angina pectoris) |
|
|
Arrhythmias (including bradycardias, ventricular tachycardias and atrial fibrillations) |
Very rare |
|||
|
Myocardial infarction |
Very rare |
|||
|
Palpitations |
Rare |
Rare |
||
|
Tachycardia |
Rare |
|||
|
Vascular disorders |
Hypotension |
Rare |
Rare |
Rare |
|
Orthostatic hypotension |
Rare |
|||
|
Flushing |
Rare |
Frequent |
||
|
Vasculitis |
Very rare |
|||
|
Respiratory, thoracic and mediastinal disorders |
Bronchitis |
Frequent |
||
|
Cough |
Rare |
Frequent |
Very rare |
|
|
Dyspnea |
Rare |
Rare |
||
|
Pharyngitis |
Frequent |
|||
|
Rhinitis |
Frequent |
Rare |
||
|
Gastrointestinal disorders |
Abdominal pain |
Frequent |
Frequent |
|
|
Changes in bowel movement (including diarrhea and constipation) |
Rare |
|||
|
Constipation |
Rare |
|||
|
Diarrhea |
Rare |
Frequent |
||
|
Dry mouth |
Rare |
Rare |
||
|
Dyspepsia |
Rare |
Frequent |
Rare |
|
|
Gastritis |
Very rare |
|||
|
Gastroenteritis |
Frequent |
|||
|
Gingival hyperplasia |
Very rare |
|||
|
Nausea |
Rare |
Frequent |
Frequent |
|
|
Pancreatitis |
Very rare |
|||
|
Epigastric pain |
Rare |
|||
|
Vomiting |
Rare |
Rare |
Rare |
|
|
Hepatobiliary disorders |
Increased liver enzymes |
Frequent |
Very rare (usually associated with cholestasis) |
|
|
Hepatitis |
Very rare |
|||
|
Jaundice |
Very rare |
|||
|
Skin and subcutaneous tissue disorders |
Alopecia |
Rare |
||
|
Angioneurotic edema |
Rare |
Very rare |
||
|
Allergic dermatitis |
Rare |
|||
|
Erythema multiforme |
Very rare |
|||
|
Exanthema |
Rare |
Rare |
||
|
Exfoliative dermatitis |
Very rare |
|||
|
Hyperhidrosis |
Rare |
|||
|
Photosensitivity |
Very rare |
|||
|
Pruritus |
Rare |
Rare |
||
|
Purpura |
Rare |
|||
|
Angioedema |
Very rare |
|||
|
Rash |
Rare |
Rare |
Rare |
|
|
Skin discoloration |
Rare |
|||
|
Stevens Johnson Syndrome |
Very rare |
|||
|
Urticaria |
Rare |
Rare |
Very rare |
|
|
Musculoskeletal and connective tissue disorders |
Ankle swelling |
Frequent |
||
|
Arthralgia |
Rare |
|||
|
Arthritis |
Frequent |
|||
|
Back pain |
Rare |
Frequent |
Rare |
|
|
Muscle spasms |
Rare |
Rare |
Rare |
|
|
Myalgia |
Rare |
Rare |
||
|
Pain in extremity |
Rare |
|||
|
Bone pain |
Frequent |
|||
|
Kidney and urinary tract disorders |
Acute renal failure |
Rare |
||
|
Haematuria |
Frequent |
|||
|
Increased voiding frequency |
Rare |
|||
|
Urination disorders |
Rare |
|||
|
Nocturia |
Rare |
|||
|
Pollakiuria |
Rare |
|||
|
Renal failure |
Rare |
|||
|
Urinary tract infection |
Frequent |
|||
|
Reproductive system and breast disorders |
Erectile dysfunction / impotence |
Rare |
Rare |
|
|
Gynecomastia |
Rare |
|||
|
General disorders and administration site conditions |
Asthenia |
Rare |
Rare |
Rare |
|
Chest pain |
Frequent |
Rare |
||
|
Face edema |
Rare |
Rare |
||
|
Tired |
Frequent |
Frequent |
Frequent |
|
|
Flu syndrome |
Frequent |
|||
|
Lethargy |
Rare |
|||
|
Discomfort |
Rare |
Rare |
||
|
Edema |
Frequent |
Frequent |
||
|
Pain |
Frequent |
Rare |
||
|
Peripheral edema |
Frequent |
Frequent |
||
|
Edema taking the scoop |
Frequent |
|||
|
Investigations |
Hypercreatininaemia |
Rare |
Rare |
|
|
Increased blood creatine phosphokinase |
Frequent |
|||
|
Hypokalaemia |
Rare |
|||
|
Increased blood urea |
Frequent |
|||
|
Hyperuricemia |
Rare |
|||
|
Increased gamma-GT |
Rare |
|||
|
Weightloss |
Rare |
|||
|
Weight gain |
Rare |
|||
- Isolated cases of rhabdomyolysis have been reported with combinations comprising angiotensin II receptor antagonists. Isolated cases of extrapyramidal syndrome have been reported in patients treated with amlodipine.
AXELER Interactions
Taking other medications
Please tell your doctor or pharmacist if you are taking or have recently taken any of the following medicines:
- Potassium supplements, salt substitutes containing potassium, medicines that increase the amount of urine you make(diuretics), or heparin (to thin the blood and prevent blood clots). Using these medicines together with AXELER may increase the potassium levels in your blood.
- Lithium(a medicine used to treat mood changes and some types of depression). The use of this medicine at the same time as AXELER may increase the toxicity of lithium. If you need to take lithium, your doctor will measure your blood lithium level.
- Nonsteroidal anti-inflammatory drugs(NSAIDs, medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis). Using these medicines together with AXELER may increase the risk of kidney failure. The effect of AXELER may be reduced by NSAIDs.
- Other blood pressure lowering medicines, the use of which may increase the effect of AXELER.
- Certain antacids(treatment for heartburn or indigestion), the use of which may slightly decrease the effect of AXELER.
- Medicines used in HIV / AIDS(eg: ritonavir, indinavir, nelfinavir) or the treatment of yeast infections (eg: ketoconazole, itraconazole).
- Diltiazem, verapamil(substances used in arrhythmias and high blood pressure).
- Rifampicin, erythromycin, clarithromycin (substances used in tuberculosis or other infections).
- John’s Wort (Hypericum perforatum) extract, (herbal remedy).
- Dantrolene(infusion for severe increases in body temperature).
- Simvastatin, asubstance used to lower the levels of cholesterol and fats (triglycerides) in the blood.
If you are taking or have recently taken any other medicines, including medicines obtained without a prescription, talk to your doctor or pharmacist.
INTERACTIONS OF AXELER 40 MG / 10 MG WITH FOOD AND DRINK
Food and drinks
- AXELER can be taken with or without food. Swallow the tablet with a liquid (such as a glass of water). If possible, take your daily dose at the same time each day, for example at breakfast time.
- Grapefruit juice and grapefruit should not be consumed by people taking AXELER. This is because grapefruit and grapefruit juice can cause increased blood levels of the active substance, amlodipine, which can cause an unpredictable increase in the antihypertensive effect of AXELER.
Drive and use machines
AXELER may have minor or moderate influence on the ability to drive and use machines. The possibility of occasional dizziness, headache, nausea or fatigue during antihypertensive treatment, which may decrease the ability to respond, should be taken into account. Caution is recommended especially at the start of treatment.
Warnings and Precautions
Take special care with AXELER 40 mg / 10 mg film-coated tablets:
Before taking these tablets, tell your doctor if you have any of the following:
- Kidney problems or kidney transplant.
- Liver disease.
- Heart failure or problems with your heart valves or heart muscle.
- Severe vomiting, diarrhea, high dose treatment with medicines that increase the amount of urine you make (diuretics) or if you are on a low salt diet.
- High levels of potassium in your blood.
- Problems with your adrenal glands (hormone-producing glands above the kidneys).
As with any medicine that lowers blood pressure, an excessive drop in blood pressure in patients with blood flow disturbances to the heart or brain can lead to a heart attack or stroke. Your doctor should therefore carefully check your blood pressure.
You must tell your doctor if you think you are (or might become) pregnant. AXELER is not recommended in early pregnancy and should not be taken if you are more than 3 months pregnant, as it could seriously harm your child if used from this stage of pregnancy.
Children and adolescents
- AXELER is not recommended for children and adolescents under 18 years old.
Older subjects
- If you are over 65, your doctor should check your blood pressure regularly with each dose increase to make sure that your blood pressure is not getting too low.
Black patients
- As with other similar medicines, the effect of AXELER in lowering blood pressure may be somewhat weaker in black patients.
PREGNANCY & BREAST-FEEDING & FERTILITY
Pregnancy
( see section Contraindications )
- There are no data from the use of AXELER in pregnant women. Animal reproduction toxicity studies have not been performed with AXELER.
Olmesartan medoxomil (active ingredient in AXELER)
- The use of angiotensin II receptor antagonists is not recommended in the 1st trimester of pregnancy . The use of angiotensin II receptor antagonists is contraindicated in the 2nd and 3rd trimester of pregnancy ( see sections Contraindications and Warnings and precautions for use ).
- The available epidemiological data concerning the risk of malformation after exposure to ACE inhibitors in the 1st trimester of pregnancy do not allow a conclusion. However, a small increase in the risk of birth defects cannot be excluded. There are no controlled epidemiological studies available concerning the use of ARBs in the 1st trimester of pregnancy, however a risk similar to that of ACE inhibitors could exist for this class. Unless treatment with ARAII is considered essential, it is recommended in patients planning to become pregnant to change antihypertensive therapy to a medicine with an established safety profile during pregnancy. If pregnancy is diagnosed, treatment with ARAII should be stopped immediately and, if necessary,
- Exposure to ARAII during the 2nd and 3rd trimesters of pregnancy is known to cause fetotoxicity (decreased renal function, oligohydramnios, delayed ossification of the skull bones) and toxicity in the newborn (renal failure , hypotension, hyperkalaemia) ( see section Preclinical safety data ).
- In case of exposure from the 2nd trimester of pregnancy, it is recommended to do a fetal ultrasound in order to check the renal function and the bones of the vault of the skull. Newborns whose mothers have taken angiotensin II receptor antagonists should be closely observed for hypotension because of the risk of hypotension ( see sections Contraindications and Warnings and Precautions ).
Amlodipine (active ingredient in AXELER)
- Data available from a limited number of pregnancies exposed to amlodipine or other calcium channel blockers do not indicate any adverse effects on the health of the fetus. However, there is a risk of prolonged childbirth.
- Therefore, AXELER is not recommended during the 1st trimester of pregnancy and contraindicated in the 2nd and 3rd trimesters of pregnancy ( see sections Contraindications and Warnings and precautions for use ).
Feeding with milk
- Olmesartan is excreted in the milk of lactating rats. However, it is not known whether olmesartan is excreted in human milk. Amlodipine is excreted in breast milk. The proportion of the maternal dose received by the infant has been estimated by an interquartile range of 3-7%, with a maximum of 15%. The effect of amlodipine on infants is unknown During breast-feeding, AXELER is not recommended and it is preferable to use other treatments with a well-established safety profile during breast-feeding, especially in newborns or babies. the premature.
Fertility
- Reversible biochemical changes in the sperm head have been reported in some patients treated with calcium channel blockers. There is insufficient clinical data regarding the potential effect of amlodipine on fertility. In a study in rats, adverse effects were detected on male fertility (see section Preclinical safety data).
- What happens if I overdose from AXELER?
- If you take more AXELER 40 mg / 10 mg film-coated tablet than you should:
- If you take more tablets than you should your blood pressure may become low and you may experience symptoms such as dizziness; a slow or fast heartbeat.
- If you take more tablets than you should or if a child accidentally swallows them, go to your doctor or nearest emergency department immediately and take the medicine pack or this leaflet with you.
What should I do if I miss a dose?
If you forget to take AXELER 40 mg / 10 mg film-coated tablets:
If you forget to take a dose, take the next dose at the usual time. Do not take a double dose to make up for the dose you forgot to take.
What is Forms and Composition ?
Forms
- Coated tablet.
- 8 mm, cream, round film-coated tablet marked with “C75” on one side.
14, 28, 30, 56, 90, 98, 10 × 28 and 10 × 30 film-coated tablets in blisters (Polyamide / Aluminum / PVC / Aluminum)
10, 50 and 500 film-coated tablets in individual blisters (Polyamide / Aluminum / PVC / Aluminum)
Not all presentations may be marketed.
Other shapes
- AXELER 20 mg / 5 mg, film-coated tablet, box of 30
- AXELER 20 mg / 5 mg, film-coated tablet, box of 90
- AXELER 40 mg / 10 mg, film-coated tablet, box of 30
- AXELER 40 mg / 10 mg, film-coated tablet, box of 90
- AXELER 40 mg / 5 mg, film-coated tablet, box of 90
Composition
| Active ingredient | Coated tablet |
|---|---|
| Olmesartan medoxomil | 40 mg * |
| Amlodipine | 10 mg * |
* per unit dose
Excipients: Tablet core: Pregelatinized corn starch , Croscarmellose sodium , Magnesium stearate , Silicified microcrystalline cellulose : Microcrystalline cellulose with , Colloidal anhydrous silica , Film coating: Polyvinyl alcohol , Macrogol 3350 , Talc , Titanium dioxide , Iron oxide yellowNo excipient with known effect ? is not present in the composition of this drug
NOT’s
Edrug-online contains comprehensive and detailed information about drugs available in the medical field, and is divided into four sections:
general information:
- Includes a general description of the drug, its use, brand names, FAQs, and relevant news and articles
Additional information:
- General explanation about dealing with the medicine: how to take the medicine, the doses and times of it, the start and duration of its effectiveness, the recommended diet during the period of taking the medicine, the method of storage and storage, recommendations in cases for forgetting the dose and instructions to stop taking the drug and take additional doses.
Special warnings:
- For pregnant and breastfeeding women, the elderly, boys and drivers, and use before surgery.
Side effects:
- It treats possible side effects and drug interactions that require attention and its effect on continuous use.
- The information contained in this medicine is based on medical literature, but it is not a substitute for consulting a doctor.
from Drug Online https://bit.ly/3dNrbtg
via Edrug Online
from faculty of medicine https://bit.ly/3jl7qKW
via Faculty of Medicine
Comments
Post a Comment